Gingivitis- Introduction, Classification, Stages and Clinical Features | Periodontics Lectures | Dental Notes
INTRODUCTION
- Inflammation of the gingiva is called gingivitis.
- Gingivitis is usually mild and does not cause destruction of the attachment fibers and underlying bone.
- Untreated gingivitis can progress to serious periodontal diseases.
CLASSIFICATION
1) ACCORDING TO DURATION
ACUTE GINGIVITIS- Sudden in onset, Short in duration and Painful in nature.
CHRONIC GINGIVITIS- Slow in onset, Long in duration and Mostly Painless. Most common type of gingivitis.
2) ACCORDING TO DISTRIBUTION
$ads={2}
LOCALIZED GINGIVITIS- Gingivitis when confined to the gingiva of a single tooth or group of teeth.
GENERALIZED GINGIVITIS- Gingivitis which involves the entire gingiva of the mouth.
MARGINAL GINGIVITIS- It involves the gingival margin and may include a portion of the contiguous attached gingiva.
PAPILLARY GINGIVITIS- Gingivitis which mainly involves the interdental papillae and may extends into the adjacent portion of the gingival margin.
DIFFUSE GINGIVITIS- It affects the gingival margin, interdental papillae and attached gingiva.
STAGES OF GINGIVITIS
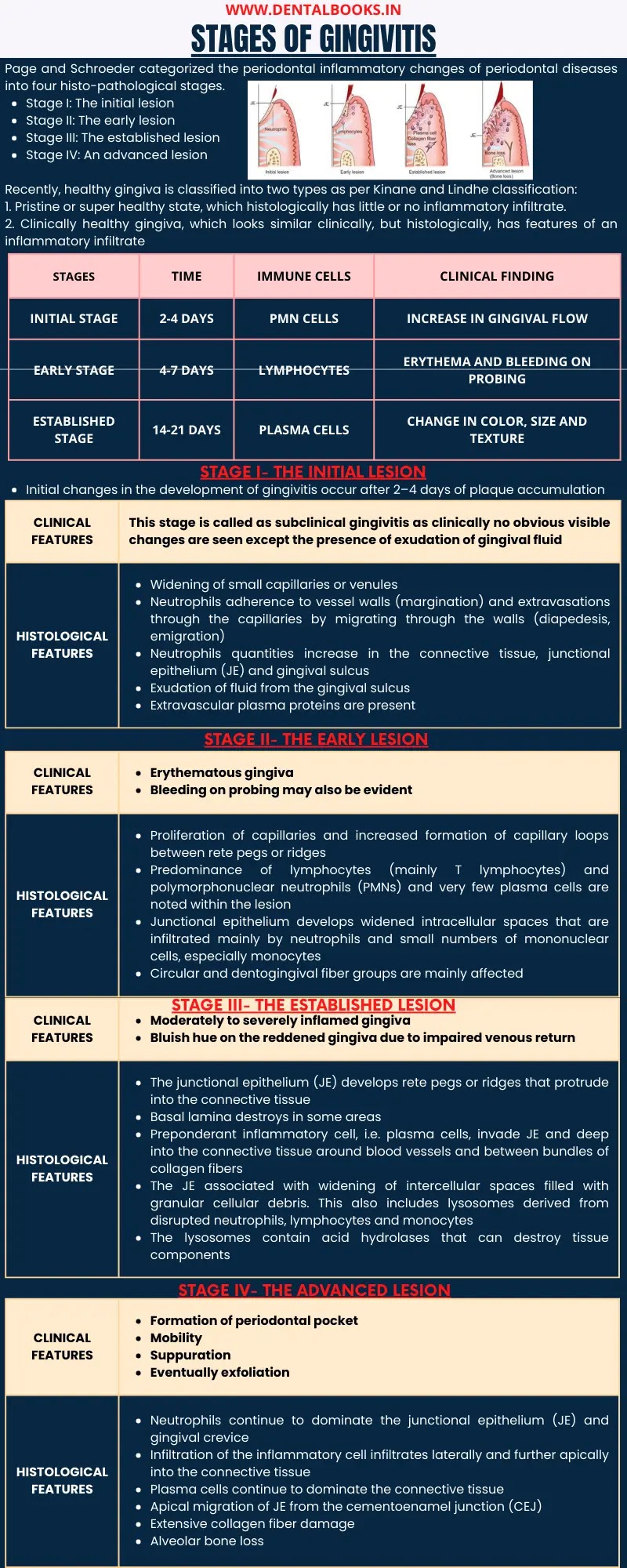
Page and Schroeder categorized the periodontal inflammatory changes of periodontal diseases into four histo-pathological stages.
Stage I: The initial lesion
Stage II: The early lesion
Stage III: The established lesion
Stage IV: An advanced lesion
Recently, healthy gingiva is classified into two types as per Kinane and Lindhe classification:
1. Pristine or super healthy state, which histologically has little or no inflammatory infiltrate.
2. Clinically healthy gingiva, which looks similar clinically, but histologically, has features of an inflammatory infiltrate
| STAGES | TIME | IMMUNE CELLS | CLINICAL FINDING |
| INITIAL STAGE | 2-4 DAYS | PMN CELLS | INCREASE IN GINGIVAL FLOW |
| EARLY STAGE | 4-7 DAYS | LYMPHOCYTES | ERYTHEMA AND BLEEDING ON PROBING |
| ESTABLISHED STAGE | 14-21 DAYS | PLASMA CELLS | CHANGE IN COLOR, SIZE AND TEXTURE |
STAGE I: THE INITIAL LESION
Initial changes in the development of gingivitis occur after 2–4 days of plaque accumulation.
| CLINICAL FEATURES |
|
| HISTOLOGICAL FEATURES |
|
STAGE II: THE EARLY LESION
| CLINICAL FEATURES |
|
| HISTOLOGICAL FEATURES |
|
STAGE III: THE ESTABLISHED LESION
| CLINICAL FEATURES |
|
| HISTOLOGICAL FEATURES |
|
STAGE IV: THE ADVANCED LESION
| CLINICAL FEATURES |
|
| HISTOLOGICAL FEATURES |
|
CLINICAL FEATURES
GINGIVAL BLEEDING
Gingival bleeding is one of the earliest symptoms of gingival inflammation
Pathogenesis of Gingival Bleeding- It is mainly due to the dilation and engorgement of capillaries. Degradation of intercellular cementing substances and widening of intercellular spaces leads to increase in the permeability of the sulcular epithelium. As the inflammation becomes chronic, ulceration of sulcular epithelium takes place.
Significance of Gingival Bleeding- Clinically, gingival bleeding can be easily noticed on probing. Hence, it is very significant for the early diagnosis and prevention of advanced gingivitis. It is a more objective sign and therefore requires less subjective estimation by the examiner.
CHANGE IN GINGIVAL COLOR
Normally, gingiva is coral pink in color due to the vascular supply and modified by overlying keratinized layer. With increase in vascularization and reduction of keratinization, the gingiva turns into red. Gingival color changes depend mainly on intensity of the inflammation.
CHANGE IN GINGIVAL CONTOUR
Normally, the contour of marginal gingiva is scalloped and knife-edged.
Interdental papilla is pointed and pyramidal in anterior region whereas in posterior region it is tentshaped, filling the area.
Conditions in which gingival contour is altered are as follows:
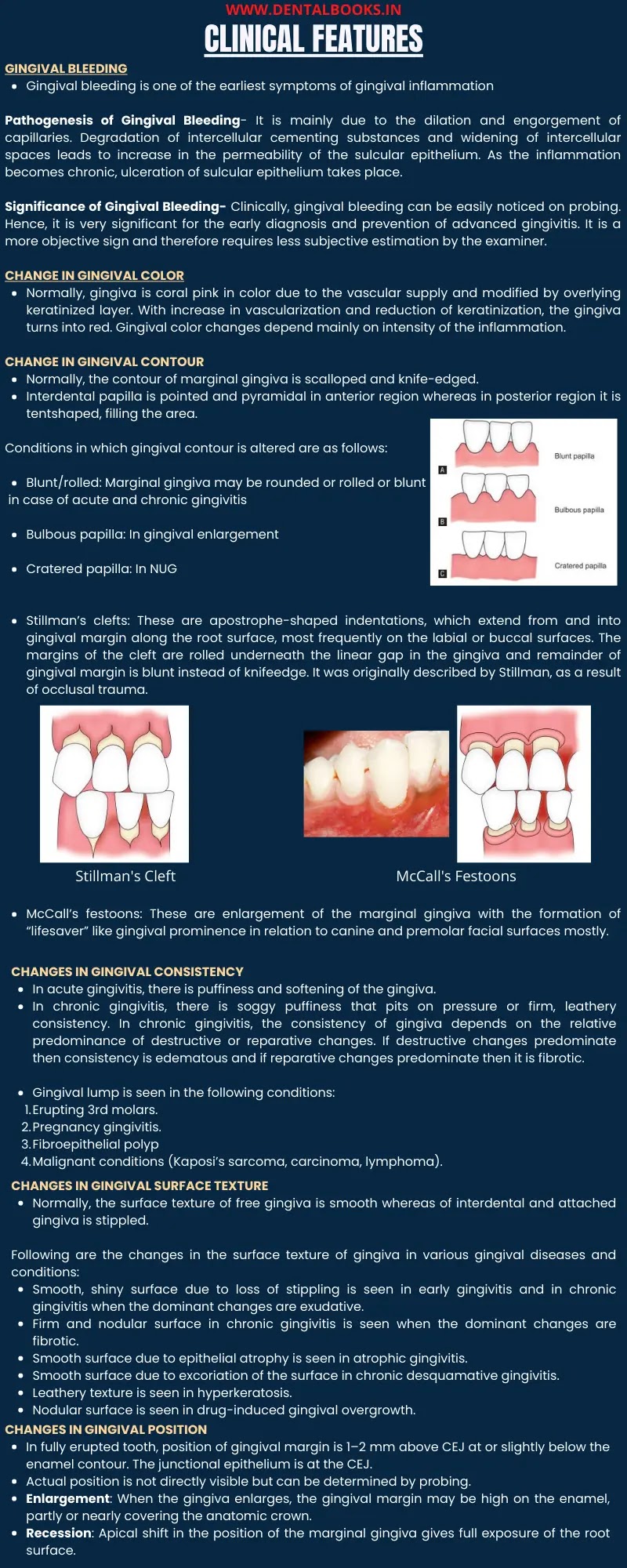
- Blunt/rolled: Marginal gingiva may be rounded or rolled or blunt in case of acute and chronic gingivitis
- Bulbous papilla: In gingival enlargement
- Cratered papilla: In NUG
- Stillman’s clefts: These are apostrophe-shaped indentations, which extend from and into gingival margin along the root surface, most frequently on the labial or buccal surfaces. The margins of the cleft are rolled underneath the linear gap in the gingiva and remainder of gingival margin is blunt instead of knifeedge. It was originally described by Stillman, as a result of occlusal trauma.
- McCall’s festoons: These are enlargement of the marginal gingiva with the formation of “lifesaver” like gingival prominence in relation to canine and premolar facial surfaces mostly.
CHANGES IN GINGIVAL CONSISTENCY
In acute gingivitis, there is puffiness and softening of the gingiva.
In chronic gingivitis, there is soggy puffiness that pits on pressure or firm, leathery consistency. In chronic gingivitis, the consistency of gingiva depends on the relative predominance of destructive or reparative changes. If destructive changes predominate then consistency is edematous and if reparative changes predominate then it is fibrotic.
Gingival lump is seen in the following conditions:
- Erupting 3rd molars.
- Pregnancy gingivitis.
- Fibroepithelial polyp
- Malignant conditions (Kaposi’s sarcoma, carcinoma, lymphoma).
CHANGES IN GINGIVAL SURFACE TEXTURE
Normally, the surface texture of free gingiva is smooth whereas of interdental and attached gingiva is stippled.
Following are the changes in the surface texture of gingiva in various gingival diseases and conditions:
- Smooth, shiny surface due to loss of stippling is seen in early gingivitis and in chronic gingivitis when the dominant changes are exudative.
- Firm and nodular surface in chronic gingivitis is seen when the dominant changes are fibrotic.
- Smooth surface due to epithelial atrophy is seen in atrophic gingivitis.
- Smooth surface due to excoriation of the surface in chronic desquamative gingivitis.
- Leathery texture is seen in hyperkeratosis.
- Nodular surface is seen in drug-induced gingival overgrowth.
CHANGES IN GINGIVAL POSITION
In fully erupted tooth, position of gingival margin is 1–2 mm above CEJ at or slightly below the enamel contour. The junctional epithelium is at the CEJ.
Actual position is not directly visible but can be determined by probing.
Enlargement: When the gingiva enlarges, the gingival margin may be high on the enamel, partly or nearly covering the anatomic crown.
Recession: Apical shift in the position of the marginal gingiva gives full exposure of the root surface.
.webp)